The main characteristic of fictitious disorders is the presence of intentional or simulated physical or psychological symptoms, this diagnosis can be made by simple direct observation or excluding other causes, although in many cases it remains controversial because it is never possible to rule out 100% that the patient does not actually present the symptoms.
The person claims that these symptoms assume the role of a patient, however, it does not seek any benefit. This sets it apart from the acts of simulation, in the simulation the patient also intentionally produces the symptoms, but its objective is easily recognized when its circumstances are known.
- For example.
- The production of symptoms intentionally to avoid a court hearing or.
- In the past.
- When filing was mandatory for military service.
- Similarly.
- A patient hospitalized for a mental disorder can simulate an aggravation of his illness to prevent his transfer to another less desirable institution.
- It would also be an act of simulation.
On the other hand, in the fictitious disorder, there is a psychological need to assume the role of the patient, as evidenced by the absence of external incentives.
By definition, the diagnosis of a fictitious disorder always involves a certain degree of psychopathology (in other words, something is wrong with that person’s mind) It should be noted that the presence of fictional symptoms does not exclude the existence of other physical or psychological symptoms. symptoms As we have seen before, in many cases the issue is complicated.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) includes the following criteria for the psychologist or psychiatrist to diagnose the dummy disorder:
DSM-IV also performs the following classification of fictitious disorders:
As we have said, the essential feature of this disorder is the intentional production of physical or psychological signs or symptoms, symptoms that can be invented (for example, when the patient complains of pain in the abdomen without being really sick) or counterfeit (for example, in the case of an abscess produced by injecting saliva under the skin).
Symptoms can also be an exaggeration or exacerbation of a pre-existing physical disorder (for example, simulation of delusions when there is a history of psychotic disorder). In addition, symptoms can be a combination or variation of all of the above.
People with this disorder often tell their story with an overly dramatic staging and air, however, if more details are asked for their answers will be vague and inconsistent, these people often get carried away by a tendency to lie that is beyond their control. . Your lies are pathological. These lies attract the interviewer’s attention and refer to any aspect of their story or symptoms.
These people usually have a deep knowledge of medical terminology and the work done in hospitals, their complaints often include problems such as pain and the need to take painkillers, when the doctor explores their physical discomfort and the result is negative, they begin to complain . other physical problems and create more fictional symptoms.
People with a dummy disorder are usually subjected to multiple scans and surgeries, but instead, when they’re in the hospital, they usually don’t get many visits.
Sometimes it is possible to surprise the person when their fictitious symptoms appear; when she realizes that she has been caught lying, denies or quickly leaves the hospital, even against the advice of a doctor; many times they are admitted to another hospital on the same day.
This subtype of dummy disorder is a clinical picture in which psychological signs and symptoms predominate. The main symptoms are the intentional production or claim of psychological symptoms, evocative of a mental illness. The apparent objective of the individual is to assume the role of “patient on the other hand, it is not understandable in the light of their environmental circumstances (unlike in the simulation).
The disorder is often recognized by a wide range of symptoms that often do not correspond to a typical symptomatic pattern; these symptoms have a clinical evolution and an unusual therapeutic response; worsen when the person knows they are being watched. He often complains of depression and suicidal thoughts due to the death of the spouse (which is not confirmed by family members), memory loss, hallucinations or delusions, symptoms of post-traumatic stress disorder, and dissociative symptoms.
On the contrary, they can also be extremely negative and un cooperative with the interview with the doctor. Psychological symptoms usually reveal the concept that the patient has a mental illness and therefore cannot match any of the known diagnostic categories.
This type consists of a clinical picture in which the signs and symptoms of an apparent physical illness Predominate The common clinical problems simulated or caused are infections (p. E. g. Abscesses), difficulty curing wounds, pain, hypoglycemia, anemia, bleeding, rashes, neurological symptoms, vomiting, diarrhea, fever of unknown origin and symptoms of autoimmune or connective tissue disorders.
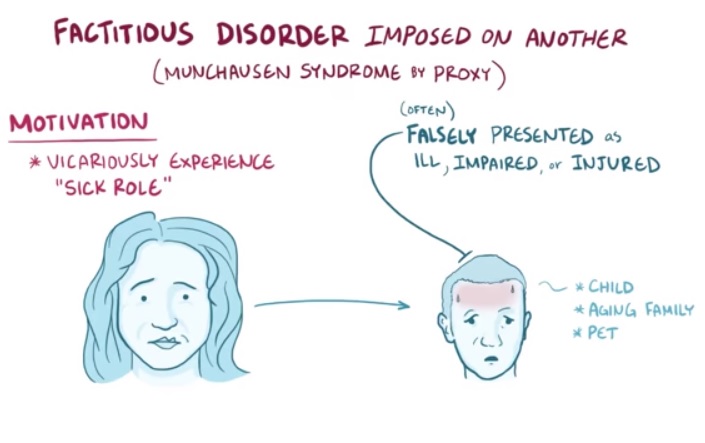
The most severe and chronic form of this disorder was called ”M nchausen syndrome”. The syndrome consists of repeated hospitalization, a pilgrimage (travel) and a fantastic pseudology. All organic systems are potential targets and the presentation of symptoms is limited only by the medical knowledge, sophistication and imagination of the individual.
This subtype consists of a clinical picture in which a combination of psychological and physical signs and symptoms appears, but none predominate over the other; the most severe and chronic form of this disorder is called ‘Mnchausen syndrome’, which we referred to above, but with the combination of the symptoms mentioned above.
The course of the dummy disorder is intermittent episodes. Less common is a single episode or chronic disease that does not improve. The onset of the disease occurs in the early years of adulthood. This often coincides with hospitalization for a physical illness or identifiable mental disorder.
In the chronic form of the disorder, successive hospitalizations almost become a lifestyle.