Schizophrenia is a complex disorder that affects approximately 1% of the world’s population, being one of the most important causes of chronic disability, although there is currently no high degree of agreement regarding its etiology, in recent years it has been linked to changes in glutamatergic. neurotransmission, so the glutamatergic hypothesis of schizophrenia remains a new approach to the cause and possible treatment of this mental illness, the protagonist of which is the glutamate mechanism.
This hypothesis focuses on the failure of a neurotransmitter called glutamate. The process that occurs is a hypofunction of glutamate. To better understand the mechanism of this neurotransmitter in schizophrenia, it is important to know how schizophrenia works and what schizophrenia is. Let’s go further.
Excess glutamate acts on different receptors by activating neurotoxic processes.
Glutamate is one of the main neurotransmitters of the nervous system, it is responsible for 80% of the energy consumed by our brain, in addition it participates in certain processes of metabolism, antioxidant production, motor and sensory systems, emotions and behavior. .
This neurotransmitter acts by mediating excitatory responses and is involved in neuroplasticity processes, i. e. in the ability to adapt our brain as a result of a certain experience, also participates in learning processes and is linked to other neurotransmitters such as GABA and dopamine.
When glutamate is released by synaptic vesicles, it activates different pathways; In addition, this neurotransmitter is associated with another, GABA, its precursor, which works by disabling glutamate-activated pathways and is therefore glutamate antagonist.
On the other hand, glutamate is involved in cognitive, memory, motor, sensory and emotional information, it is no coincidence that we begin to study its relationship with schizophrenia, considering its cognitive and behavioral functioning.
Schizophrenia is a serious mental disorder that greatly affects a person’s quality of life, according to the current statistical manual and the diagnosis of mental disorders the following symptoms usually appear:
To be schizophrenic, two or more of the previous symptoms must be present within a month or less if treated correctly and continuous signs of deterioration should also persist for at least 6 months. There must also be a deterioration in the functioning of one or fewer more important areas (work, relationships, personal care).
On the other hand, the disease is excluded when these symptoms are due to the effects of a substance. In addition, if there is a history of autism spectrum disorder, schizophrenia is diagnosed only if hallucinations and delusions are severe.
The glutamatergic hypothesis was created to try to address the growing need to find a theory that explains this disease, because although there are some theories, they were not enough to understand the mechanism of schizophrenia.
Thus, at first, the cause of schizophrenia was considered a dopamine-related problem; later, researchers realized that glutamate plays a fundamental role, in addition to dopamine, and that it may be related to this disease, so the glutamatergic hypothesis appeared that schizophrenia is caused by a hypofunction of glutamate in cortical projections, i. e. a decrease in the normal functioning of this neurotransmitter in the cortical region of the brain.
However, the glutamatergic hypothesis of schizophrenia does not exclude the dopamine hypothesis, but proposes that in case of glutamate hypofunction an increase in dopamine intake is generated, that is, this hypothesis is a complement to dopamine theory.
Glutamate neurons generate activity in GABA interneurons, which in turn are responsible for inhibiting glutamatergic neurons. Thus, they prevent overactivation and therefore excess glutamate. This process allows not to cause neuronal death. In schizophrenia, this system is affected.
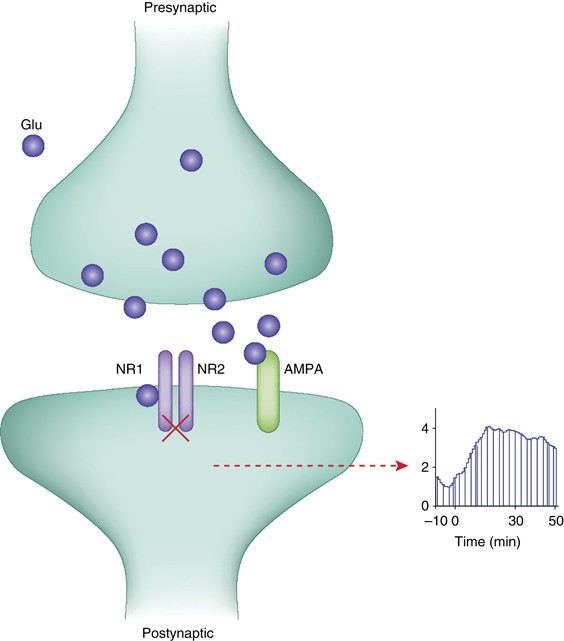
As mentioned above, the glutamatergic hypothesis is associated with glutamatergic receptor dysfunction, because in schizophrenia they generate less cortical activity and therefore contribute to the onset of certain symptoms, that is, when glutamatergic receptors do not play the role they are supposed to play, this disorder appears.
The importance of these receptors was discovered when substances were administered intravenously that blocked them and, in turn, caused cognitive and behavioral symptoms similar to those in schizophrenia.
In contrast, receptors that have glutamate and have also been studied in schizophrenia are:
It should be noted that, while there are specific results, there are other contradictory results. The most frequently studied onotropic receptors that show better results are NMDA. The action of AMPA and kainato receptors has also been studied, but the results are non-consolidated.
In addition, when NMDA receptors do not work well, they cause neuronal death and therefore behavioral disorders typical of schizophrenia. For AMPA and Kanate receptors, consistent data from different authors is required for the information to be considered relevant.
In contrast, metabotropic receptors are associated with neural protection, when modified decreases the action of glutamate, thus causing behavioral problems typical of schizophrenia, in addition, several studies address the therapeutic scope of schizophrenia.
Apart from the glutamatergic hypothesis, pharmacological substances have been created that attempt to mimic the role of glutamate receptors, and apparently good results have been obtained experimentally.
However, this does not mean that the process is simple or that the treatment is effective, controlling the activation of the receptors is not easy and overactivation can be harmful, in addition, since the studies focus on global symptoms, not areas, and most have been done in animals, we cannot be sure of the exact relationship between a symptom and the location of the brain in humans.
The glutamatergic hypothesis is a breakthrough, but it should not be forgotten that in schizophrenia not only biological but also environmental factors occur, future research could combine several aspects to better understand this disorder, perhaps a holistic approach is good for understanding all the factors associated with this disorder.