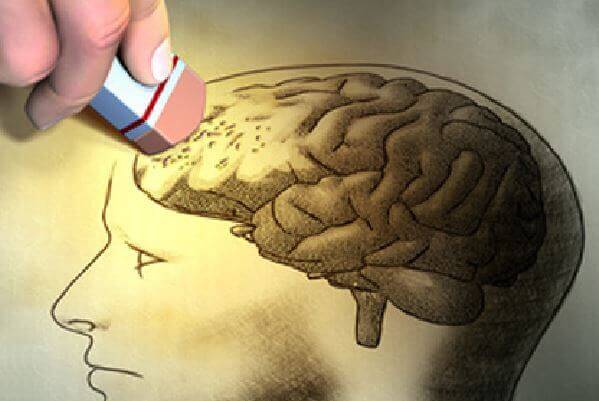
The shape or position we sleep in could have an effect on our neurological health, according to a study by Stony Brook University in the United States. Apparently, sleeping sideways or sideways would help our brain remove certain wastes that contribute to the increased risk of Alzheimer’s and Parkinson’s, among other diseases.
Although these findings are still isolated discoveries, they open up a broad line of research to determine what caused them and what kind of preventive advice can be given directly to the population to reduce the risk of these diseases. While the conclusions are complex, we can learn from them. So, let’s see how the study unfolded.
- An international team of scientists led by researchers at Stony Brook University has discovered that sleeping sideways helps rat brains in their experiment to remove chemical waste from the brain through their cleaning system (glyphic system).
Using functional MRI images, researchers were able to observe how cerebrospinal fluid residues were filled with amyloid proteins and TAF, substances that, when accumulated, appear to be directly related to increased risk of Alzheimer’s and Parkinson’s.
For example, these tests revealed that the brain cleansing system was much more effective in the lateral position than in a lying position (face up) or lying down (face down).
It is curious that, apparently, this position is more common at bedtime, both in human and animal populations, in fact few people sleep with their mouths up or down, so it seems that using this strategy is a matter of naturalness. Adaptation.
So, although these findings have not yet been replicated in humans, the results are promising, because with this discovery, we know more about the biology of restful sleep function and how we can use it to reduce the risk of Alzheimer’s and Parkinson’s.
The two diseases share, in a way, a histopathological characteristic: the presence of neural and biochemical residues in the brains of patients, however, each disease is very plural in many ways, let’s look at some details about them:
It is estimated that around 2% to 5% of the population over the age of 65 suffer from Alzheimer’s dementia; this percentage is much higher (25%) 80 and reaches 30% among those over 90; in any case, the appearance can occur in a very large age group, between the ages of 40 and 90.
However, the definitive diagnosis can only be confirmed after death, as during autopsies, the brains of people with this disease have fewer cortical neurons, a large amount of senial plaques, neurofibrillary and granulovascular degeneration and an increasing accumulation of lipofuscin.
Its onset is insidious and tends to manifest itself both by short-term changes in memory and by lack of concentration and disorientation, so personality changes can also occur, so that the person is apathetic, selfish, rude, uned educated, irritable, aggressive. or stiff while in his life it was quite the opposite.
In addition to what was discovered in the study we talked about, we should consider other types of risk factors associated with the development of the disease, since controlling them can help us delay and even prevent their onset:
Factors associated with lower risk have also been identified: high educational level, staying physically and mentally active (mens sana in corpore sano) through participation in leisure activities, regular physical exercise and following a Mediterranean diet rich in antioxidants.
Although the causes are unknown, there are many hypotheses, but some can only identify or explain a portion of the cases. The genetic hypothesis, for example, covers only about 5% of cases.
Other conjectures lead to the possible influence of slow viruses or acetylcholine deficiency. High and toxic levels of metals, such as aluminum and silicon, have also been found in the brains of these patients.
Parkinson’s disease is a slow and progressive neurological disease characterized by tremors, stiffness, slow movements and postural instability.
Its main brain damage is at the level of the central gray nuclei, the structure responsible for controlling movement, among other functions. In the autopsies of these patients, obvious signs of neuronal body loss and Lewy were found in the dark substance.
Such is the interrelationship between dementias, that in the autopsies of some people with Parkinson’s disease signs of Alzheimer’s disease or Lewy body disease have been found.
As for Parkinson’s disease, it should be noted that about 30% of cases develop dementia, the onset of dementia is usually late (from age 70) and the prevalence is higher in men than in women.
Dementia associated with Parkinson’s disease often begins to manifest through difficulties in distinguishing the shape, location or position of objects, difficulty speaking fluently and, of course, changes in memory (in this case, one can begin to forget both as a bicycle and in the conversation that took place 30 minutes ago)
Risk factors are similar to those of Alzheimer’s disease, which once again demonstrates how important it is to maintain a healthy lifestyle and a balance between our mental and physical health.
So, while sleeping by your side is not yet a clearly proven preventive strategy, isn’t it an exaggeration to consider this knowledge to take care of you on a daily basis, is it surprising that with this simple gesture we can reduce the risk of Alzheimer’s and Parkinson’s?