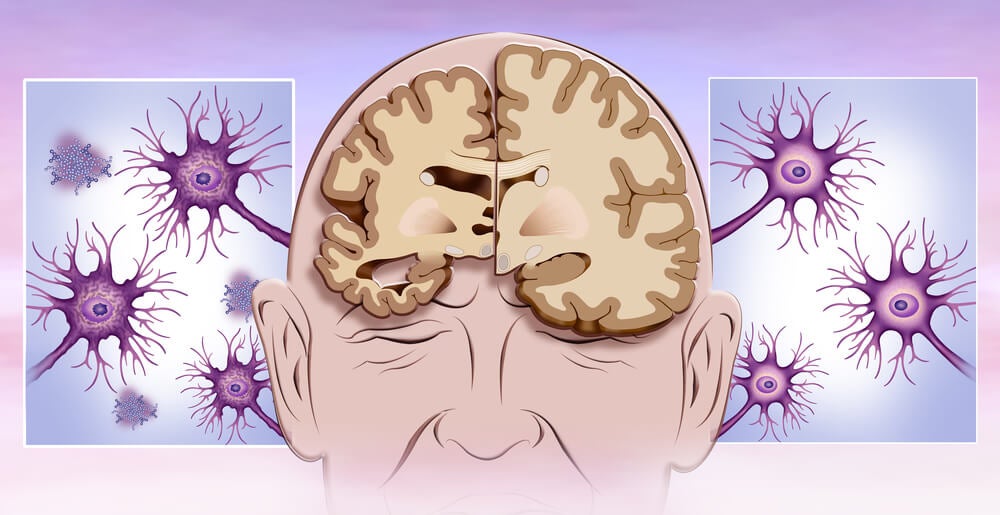
Alzheimer’s disease is the most common cause of dementia; impairment of cognitive function appears to be at the heart of cognitive symptoms of the disease; however, other symptoms can play an important role, including delirium.
This neurocognitive disorder is characterized by changes in cognition and attention, which is usually the result of a medical complication, in addition, Alzheimer’s disease is a degenerative process characterized by the loss of cholinergic neurons, essential for the proper functioning of the brain.
- Delirium is a clinical disorder that affects attention and cognition.
- However.
- Its physiopathology is little known.
- Although cognitive decline and dementia are systematically identified as the main risk factors for delirium (2.
- 3).
- The mechanisms that contribute to this increased risk remain unknown.
According to a study published in 2009, the presence of delusions is a condition that can affect cognition. Therefore, this occurs in approximately 66% to 89% of patients with Alzheimer’s disease. So it looks like these two diseases can go hand in hand.
This study shows that delusions in Alzheimer’s disease accelerate the trajectory of cognitive decline in hospitalized patients.
Pathologically, delirium is the result of diffuse brain dysfunction. Apparently, there are several causes for illusion. Authors Blass and Gibson combine these causes into two possibilities:
Drug poisoning is often a cause of delirium. However, it seems that many of the conditions that can cause delirium tend to cause dementia if they continue. For example, hypoxia or hypoglycemia can cause brain dysfunction and delusions. But if they are severe and prolonged, they can cause permanent brain damage and dementia [5].
Currently, delirium and dementia are classified as different processes, however, between the 1930s and 1970s different forms or stages of the same process were considered, for example, in 1959, Egel and Romano (1) wrote:
“As with the most common types of organic insufficiency, [brain failure] refers to what evolves when it interferes with organ function as a whole, for any reason. Can this be reduced to two underlying processes, metabolic process failure?Or the loss [of functional units] by death?Does delirium refer to the most reversible disorder and dementia to the irreversible disorder?Should these states be considered as different grades?
Thus, it could be said that delirium and Alzheimer’s disease are associated with a reduction in brain metabolic rates; In addition, both pathologies are related to an altered cholinergic function.
In Alzheimer’s dementia, unlike delirium, there is also evidence of structural brain damage; however, if a patient mistakenly diagnosed with delirium has the pathological stigma of Alzheimer’s disease at autopsy, the diagnosis would change to Alzheimer’s disease (at least in the United States).
Cholinesarase inhibitors appear to be a treatment for delirium management as well as Alzheimer’s disease; therefore, it is the appropriate drug for delusions in Alzheimer’s disease. Cholinesarase inhibitors may be particularly useful for patients in a postoperative or other settings where delirium causes serious attention problems.
In Sweden, Dr. Bengt Winblad has already conducted pioneering studies on this possibility; however, cholinesarase inhibitors should be used with caution, as cholinergic agonists present an implicit risk of causing bronchospasm or sinus node syndrome.
In this sense, care must be taken: more studies are needed that show rigorously whether cholinergic treatment protects the brain from metabolic encephalopathies and their consequences.